The ASH 2021 meeting in December covered a variety of fascinating topics. Highlights included a thought-provoking discussion on the role of minimal residual disease (MRD) and therapeutic decision-making in multiple myeloma (MM), an interesting presentation on the familial risk of MM as well as presentations of data from several novel treatments that are in development for patients with heavily pre-treated MM.
MRD in clinical practice in MM
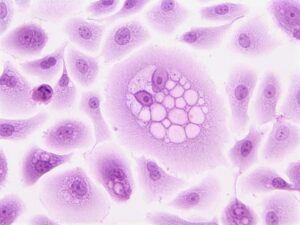
Noopur Raje, MD, was part of a panel discussion around challenges in the treatment of MM, with her focus on the prognostic value of MRD, MRD and therapeutic decision making, and MRD as a potential regulatory endpoint. A patient who has no MRD after treatment (MRD-negative) has fewer than one myeloma cell per million bone marrow cells. Patients with such low levels of residual disease are much less likely to suffer relapse compared with those with higher levels.
Dr Raje explained the need to better quantify the deep responses currently being achieved with triplet and quadruplet combinations in MM. In addition, even with the most effective treatments and a complete response with a two-fold log reduction in myeloma cells, she noted that relapse will still happen. Dr Raje suggested that “MRD is the new complete response” endpoint that was talked about 10–12 years ago.
After discussing the prognostic significance of MRD with respect to overall survival (OS) and progression-free survival (PFS), Dr Raje said that when it comes to therapeutic decision-making, not enough data yet exist to support stopping treatment in patients who are MRD-negative or administering additional treatments in patients who are MRD-positive. MRD conversion happens over time, and therefore escalation and de-escalation of treatment based on MRD should not be occurring yet, due to the paucity of supporting data. However, she expects data to emerge regarding this area in the next few years. The next big question will be when to arrange an MRD test. As well as within clinical trials, MRD testing should be considered for high-risk patients: “because it is really important to try and maintain a really deep durable response in those patients”.
Dr Raje concluded by saying that the hope is that MRD will be a potential regulatory endpoint in the very near future instead of PFS and OS as it correlates with both endpoints and could lead to quicker decisions regarding approval.
More evidence to support potential heritability of MM
Santiago Thibaud, MD, presented an elegant paper that was very well received by the audience on pathogenic/pathogenic-like germline variants (PGVs) in hereditary cancer genes (HCGs) in a cohort of 895 patients with newly diagnosed MM. A minority of cancers – generally 5–10% – are related to genetic variants (mutations) that are passed from parent to child. In this study, 83 PGVs in 31 HCGs were identified in 79 patients (9%). Patients with newly diagnosed MM and a family history of haematologic malignancies (lymphoma, leukaemia, or MM) were more likely to carry a PGV versus those without a family history (around 1:4), and PGV carriers were also much more likely to be diagnosed with MM before the age of 40 years than those without (around 1:4). In addition, those patients in whom the PGV affected the DNA-damage repair genes (DDR-PGV) that are crucial to maintaining the integrity of the genome were seen to have a longer first PFS interval (PFS1) compared with those without this type of PGV (52 vs 35 months; p=0.008).
As PGVs were relatively common in this large patient population with MM, particularly in those with a family history of haematologic malignancy or diagnosed before 40 years of age, routine screening may be warranted in high-risk patients. Such screening could focus counselling support and enrolment in early cancer detection programmes. In addition, the longer PFS1 observed in patients with DDR PGVs may be important for future clinical trial design.
Focus on novel biological therapies in patients with heavily pre-treated MM
Relapse and disease progression are inevitable for the majority of patients with MM. Repeated relapses, leading to relapsed/refractory multiple myeloma (RRMM), contribute to shorter periods of response and resistance to traditional therapies. Once patients with RRMM have experienced multiple relapses or received multiple lines of therapy (≥3) in an attempt to control their disease, they are presented with limited options for the next steps in treatment, with devastating results. Hoping to address this unique unmet need for these patients, the results of clinical studies investigating novel chimeric antigen receptor (CAR) T-cell therapies and bispecific antibodies were presented at ASH 2021.
Updated analysis of CARTITUDE-1 shows promising results
In MM, B-cell maturation antigen (BCMA) promotes the proliferation and survival of MM cells and is associated with the immunosuppression which is the hallmark of the disease. Thomas Martin, MD, presented encouraging data from an updated analysis of CARTITUDE-1, a phase Ib/II study assessing a single infusion of the BCMA-targeting CAR-T cell therapy ciltacabtagene autoleucel (cilta-cel) in patients with RRMM who had received ≥3 lines of therapy or were refractory to an IMiD, a proteasome inhibitor (PI) and an immunomodulatory drug (IMiD), and were IMiD-, PI-, and anti-CD38 antibody-exposed.
Almost every patient responded to cilta-cel (objective response rate [ORR]: 98%) and of the 61 patients evaluable for MRD, 92% were MRD-negative at the 10-5 threshold. In addition, impressive 18-month PFS and OS rates were observed (66% and 81% of patients, respectively). As well as demonstrating robust efficacy, cilta-cel also appeared to have a manageable safety profile.
Not only does cilta-cel offer hope to heavily pre-treated patients but it will also be very interesting to see what the results are in several ongoing clinical trials which are investigating cilta-cel in earlier lines of therapy.
Bispecific antibodies
Can bispecific antibodies provide a response to the issue of treatment resistance?
Bispecific antibodies, also known as bispecific T-cell engagers (BiTEs), have two binding sites, either directed at two antigens or two epitopes of one antigen. For RRMM, most bispecific antibodies in development act as immune cell connectors by linking CD3 with myeloma cells, which directs T-cell-mediated killing of myeloma cells.
In addition to BCMA-targeted CAR-T therapy, another method employed for the targeting of BCMA in RRMM is the development of bispecific antibodies which target both BCMA and CD3. REGN5458 is an example of this, and Jeffrey Zonder, MD, presented the results from the dose escalation portion of the ongoing phase I/II study investigating REGN5458 for the treatment of RRMM in patients who had received at least three lines of prior therapy.
Among all enrolled patients, the ORR was 51%, increasing to 75% in the higher dose cohort (200–800 mg). Median duration of response (DoR) was not reached. The majority of patients did not experience cytokine release syndrome (CRS), and of those who did only 3 patients (4%) experienced grade ≥2. No relationship was observed between dose level and CRS. Dose-limiting toxicities were reported in two patients and the maximum tolerated dose was not reached. Treatment-emergent adverse events (AEs) were reported in 33% of patients, most of whom experienced haematologic AEs. The promising efficacy and manageable safety profile of REGN5458 support further clinical development. The phase II portion of the study is currently recruiting.
While BCMA is a highly anticipated target for RRMM therapy, the antigen is known to shed, and this is currently being investigated to determine the impact on the efficacy of therapies, so other groups have investigated targeting stable antigens. Suzanne Trudel, MD, MSc, presented promising results from the ongoing phase I clinical study of cevostamab, a bispecific antibody that targets Fc receptor-homolog 5 (FcRH5) and CD3, for patients with heavily pre-treated RRMM. The focus of the presentation revolved around the use of cycle 1 double step-up dosing to reduce CRS without compromising efficacy.
ORR increased with target dose, from 29% in the 3.6/90 mg cycle 1 single step-up expansion cohort to 55% in the 0.3/3.6/160 mg cycle 1 double step-up cohort. Median DoR was 11.5 months in the cycle 1 single step-up expansion cohort. Rates of symptomatic grade 1 and grade 2 CRS were reduced following cycle 1 double step-up dosing, 52% vs 73% in the cycle 1 single step-up cohort. Cevostamab-related AEs were low (4%), though there was one case of cevostamab-related fatality due to haemophagocytic lymphohistiocytosis. Following the clinically meaningful activity and manageable safety profile demonstrated with cevostamab, the clinical development of cevostamab will expand over the next year.
Amrita Krishnan, MD, provided an update on the results from MonumenTAL-1, a phase I study of the G protein-coupled receptor family C group 5 (GPRC5D) and CD3 bispecific antibody, talquetamab, for patients with heavily pre-treated RRMM. Following the identification of the first recommended phase II dose (RP2D) of weekly (QW) subcutaneous (SC) doses of 405 µg/kg and the second RP2D of 800 µg/kg every two weeks (Q2W), the updated safety and efficacy data were presented.
ORR was comparable across both RP2D cohorts, 70% in the first RP2D cohort and 67% in the second RP2D cohort. Median DoR was not reached in either cohort. Rates of all grade CRS were similar for both the first and second RP2D cohort, 77% and 72%, respectively. Only one patient experienced grade ≥3 CRS. No new AEs were reported, and the majority of AEs were grade 1 or 2 in both cohorts. Both RP2D schedules provided encouraging efficacy results with a tolerable safety profile, supporting further development of talquetamab. A phase II expansion study and studies evaluating combinations of talquetamab with other agents are currently ongoing.
Can bispecific combination partners offer an alternative, effective treatment pathway?
Combination therapies are commonplace in the treatment of MM, with standard of care for patients who are newly diagnosed being the combination of an IMiD and a PI. Following multiple lines of therapy, and the development of RRMM, determining an effective and well-tolerated combination of therapies becomes trickier.
Preclinical studies have shown increases myeloma cell cytotoxicity with the addition of daratumumab, an anti-CD38 monoclonal antibody with direct on-tumour and immunomodulatory effects, to talquetamab therapy. Ajai Chari, MD, presented the interim results of the ongoing phase Ib study of daratumumab and talquetamab in patients with heavily pre-treated RRMM (TRIMM-2).
All patients received SC daratumumab 1800 mg QW for cycles 1 and 2, Q2W for cycles 3–6, with subsequent monthly treatment. Patients received SC talquetamab 400 µg/kg either QW or Q2W or 800 µg/kg Q2W, with step-up dosing. ORR ranged from 78–86% across the three treatment cohorts, which demonstrated an improvement compared with the RP2D for talquetamab monotherapy. Patients who were either CD38-exposed or CD38-refractory experienced a response. Grade 1 or 2 CRS was reported in 55% of patients, with no grade ≥3 CRS events detected. No new AEs were observed with the combination therapy compared with the single agents, with no overlapping toxicities. Skin- and nail-related disorders were reported in 65% of patients, though most were grade 1 or 2. These preliminary data suggest a promising efficacy profile with the combination therapy and safety profile consistent with those of single agents, supporting this novel immunotherapy-based combination therapy for patients with heavily pre-treated RRMM.
In summary, these ASH 2021 presentations provided valuable insights into the novel treatments being developed for a patient population for whom there are extremely limited treatment options, with palliative care often indicated in this setting. While there is still a way to go, and further clinical data required, a promising future treatment landscape exists for patients with RRMM.